BONE
Bone is the main component of the skeleton in the adult human. Like cartilage, bone is a specialised form of dense connective tissue. Bone gives the skeleton the necessary rigidity to function as attachment and lever for muscles and supports the body against gravity.
Two types of bone can be distinguished macroscopically:
- Trabecular bone
(also called cancellous or spongy bone) consists of delicate bars and sheets
of bone, trabeculae, which branch and intersect
to form a sponge like network. The ends of long bones (or epiphyses)
consist mainly of spongy bone.
- Compact bone does not have any spaces or hollows in the bone matrix that are visible to the eye. Compact bone forms the thick-walled tube of the shaft (or diaphysis) of long bones, which surrounds the marrow cavity (or medullary cavity). A thin layer of compact bone also covers the epiphyses of long bones.
 Bone is, again like cartilage, surrounded by a layer of dense connective tissue, the periosteum. A thin layer of cell-rich connective tissue, the endosteum, lines the surface of the bone facing the marrow cavity. Both the periosteum and the endosteum possess osteogenic potency. Following injury, cells in these layers may differentiate into osteoblasts (bone forming cells) which become involved in the repair of the damage to the bone.
Bone is, again like cartilage, surrounded by a layer of dense connective tissue, the periosteum. A thin layer of cell-rich connective tissue, the endosteum, lines the surface of the bone facing the marrow cavity. Both the periosteum and the endosteum possess osteogenic potency. Following injury, cells in these layers may differentiate into osteoblasts (bone forming cells) which become involved in the repair of the damage to the bone.
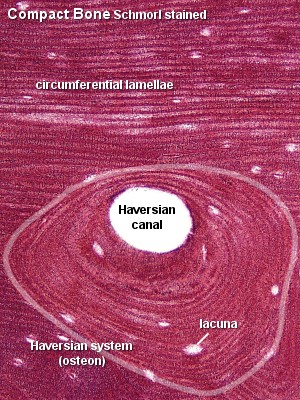
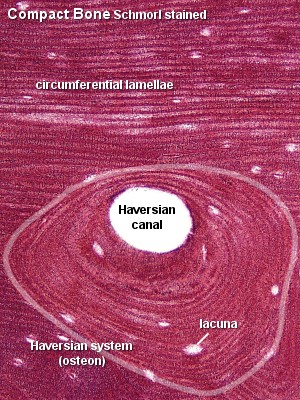
Compact Bone
Compact bone consists almost entirely of extracellular substance - the matrix. Osteoblasts deposit the matrix in the form of thin sheets which are called lamellae. Lamellae are microscopical structures. Collagen fibres within each lamella run parallel to each other. Collagen fibres which belong to adjacent lamellae run at oblique angles to each other. Fibre density seems lower at the border between adjacent lamellae, which gives rise to the lamellar appearance of the tissue. Bone which is composed by lamellae when viewed under the microscope is also called lamellar bone.
In the process of the deposition of the matrix, osteoblasts become encased in small hollows within the matrix, lacunae. Unlike chondrocytes, osteocytes have several thin processes, which extend from the lacunae into small channels within the bone, the canaliculi. Canaliculi arising from one lacuna may anastomose with those of other lacunae and, eventually, with vessel-containing canals within the bone. Canaliculi provide the means for the osteocytes to communicate with each other and to exchange substances by diffusion.
In mature compact bone most of the individual lamellae form concentric rings
around larger longitudinal canals (approx. 50 µm in diameter) within
the bone tissue. These canal are called Haversian
canals. Haversian canals typically run parallel to the surface and
along the long axis of the bone. The canals and the surrounding lamellae (8-15)
are called a Haversian system or an osteon.
A Haversian canal generally contains one or two capillaries and some nerve
fibres.
Irregular areas of interstitial lamellae, which apparently do not belong to any Haversian system, are found in between the Haversian systems. Immediately beneath the periosteum and endosteum a few lamella are found which run parallel to the inner and outer surfaces of the bone. They are the circumferential lamellae and endosteal lamellae.
A second system of canals, called Volkmann's canals, penetrates the bone more or less perpendicular to its surface. These canals establish connections with the inner and outer surfaces of the bone. Vessels in Volkmann's canals communicate with vessels in the Haversian canals on the one hand and vessels in the endosteum on the other. A few communications also exist with vessels in the periosteum.
Trabecular Bone
The matrix of trabecular bone is also deposited in the form of lamellae. In mature bones, trabecular bone will also be lamellar bone. However, lamellae in trabecular bone do not form Haversian systems. Lamellae of trabecular bone are deposited on preexisting trabeculae depending on the local demands on bone rigidity.
Osteocytes, lacunae and canaliculi in trabecular bone resemble those in compact bone.
? Note
the distinction between macroscopic (visible to the eye) and microscopic (only
visible under the microscope) appearance when the bone is named. Lamellar
bone forms both trabecular bone and compact bone, which are the two macroscopically
recognizable bone forms.
- Suitable Slides
- sections of compact bone
(usually part of the diaphysis of a long bone) - ground
(unstained), Schmorl stained or H&E
Compact Bone, human - Schmorl stain
Lamellae which run parallel to the surface of the bone are visible both on
the outer, convex surface of the bone (circumferential lamellae) and on the
inner, concave surface of the bone facing the marrow cavity (endosteal lamellae).
The surface formed by the endosteal lamellae is often more irregular than
the surface formed by the circumferential lamellae. The space between these
two sets of lamellae is filled by Haversian systems and interstitial lamellae.
Only few of the Haversian systems are "textbook" circular. Osteocyte
lacunae are visible between the lamellae. Canaliculi become visible at high
magnification (not illustrated).
You should be able to see, draw and identify Haversian
systems, interstitial and circumferential lamellae and/or endosteal lamellae.

Compact Bone, human - ground (unstained)
The osteocyte lacunae are the main feature of the ground section. They are
visible as elongated black spots in the bone matrix. Canaliculi, radiate from
the lacunae into the surrounding bone matrix. Some lamellae are visible in
the ground section. There is actually no distinct border between most lamellae,
but our brain can use the elongated osteocyte lacunae and their orientation
to "reconstruct" the lamellae.
This is one of the cases where it may pay off to close
down the iris diaphragm. The canaliculi should stand out more clearly if you
do so. Remember to open the diaphragm afterwards!
Draw a small section of the a Haversian system at high
magnification and identify in your drawing lacunae, canaliculli and (if visible)
lamellae.


- Suitable Slides
- sections of part of a vertebra or an epiphysis
of a long bone - H&E, van Gieson
Sections prepared to show articular cartilage
will often also contain trabecular bone in the epiphysis below the articular
cartilage.
Articular Cartilage, bovine - H&E
Thin sheets and bars of bone, trabeculae, are visible at low magnification.
Although they may appear as individual pieces in sections, they form an interconnected
meshwork in the living bone. The spaces between the trabeculae, the marrow
cavity of the diaphysis, is filled by either red bone marrow or yellow bone
marrow. At high magnification, elongated osteocyte lacunae, which in well
preserved tissue still contain osteocytes, are visible in the matrix. If the
H&E stain also turned out well, it should be visible that the matrix of
the trabecular bone is formed by lamellae. Canaliculi are present but hard
to identify in most H&E stained sections. Haversian systems are not
present in the trabeculae.
In trabecular bone obtained from young individuals,
in which the bone is still growing, small areas of calcified cartilage are
occasionally seen in the bone trabeculae. They are remnants of the cartilage
scaffold on which bone matrix was deposited during the formation of the trabeculae.
With the reorganisation of bone such areas will eventually be lost.
Draw trabecular bone at high and low magnification.
Make sure that it is visible that the trabecular bone is also lamellar bone.
Include enough detail of the marrow as you think you will need to identify
this type of preparation.


Bone Matrix
Bone matrix consists of collagen fibres (about 90% of the organic substance) and ground substance. Collagen type I is the dominant collagen form in bone. The hardness of the matrix is due to its content of inorganic salts (hydroxyapatite; about 75% of the dry weight of bone), which become deposited between collagen fibres.
Calcification begins a few days after the deposition of organic bone substance (or osteoid) by the osteoblasts. Osteoblasts are capable of producing high local concentration of calcium phosphate in the extracellular space, which precipitates on the collagen molecules. About 75% of the hydroxyapatite is deposited in the first few days of the process, but complete calcification may take several months.
Bone Cells
- Osteoprogenitor cells (or stem cells of
bone)
-
are located in the periosteum and endosteum. They are very difficult
to distinguish from the surrounding connective tissue cells. They differentiate
into
- Osteoblasts (or bone forming cells).
-
Osteoblasts may form a low columnar "epitheloid layer" at sites of bone
deposition. They contain plenty of rough endoplasmatic reticulum (collagen
synthesis) and a large Golgi apparatus. As they become trapped in the
forming bone they differentiate into
- Osteocytes.
-
Osteocytes contain less endoplasmatic reticulum and are somewhat smaller
than osteoblasts.
- Osteoclasts
-
 are
very large (up to 100 µm), multi-nucleated (about 5-10 visible in
a histological section, but up to 50 in the actual cell) bone-resorbing
cells. They arise by the fusion of monocytes (macrophage precursors in
the blood) or macrophages. Osteoclasts attach themselves to the bone matrix
and form a tight seal at the rim of the attachment site. The cell membrane
opposite the matrix has deep invaginations forming a ruffled
border. Osteoclasts empty the contents of lysosomes into the extracellular
space between the ruffled border and the bone matrix. The released enzymes
break down the collagen fibres of the matrix. Osteoclasts are stimulated
by parathyroid hormone (produced by the
parathyroid gland) and inhibited by calcitonin
(produced by specialised cells of the thyroid gland). Osteoclasts are
often seen within the indentations of the bone matrix that are formed
by their activity (resorption bays or Howship's
lacunae).
are
very large (up to 100 µm), multi-nucleated (about 5-10 visible in
a histological section, but up to 50 in the actual cell) bone-resorbing
cells. They arise by the fusion of monocytes (macrophage precursors in
the blood) or macrophages. Osteoclasts attach themselves to the bone matrix
and form a tight seal at the rim of the attachment site. The cell membrane
opposite the matrix has deep invaginations forming a ruffled
border. Osteoclasts empty the contents of lysosomes into the extracellular
space between the ruffled border and the bone matrix. The released enzymes
break down the collagen fibres of the matrix. Osteoclasts are stimulated
by parathyroid hormone (produced by the
parathyroid gland) and inhibited by calcitonin
(produced by specialised cells of the thyroid gland). Osteoclasts are
often seen within the indentations of the bone matrix that are formed
by their activity (resorption bays or Howship's
lacunae).
Bones are formed by two mechanisms: intramembranous ossification (bones of the skull, part of the mandible and clavicle) or endochondral ossification.
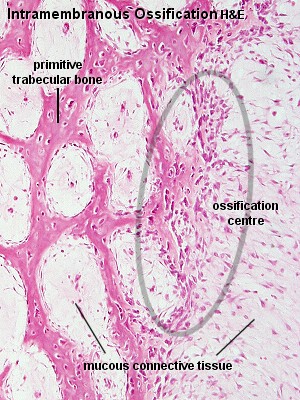
Intramembranous Ossification
Intramembranous ossification occurs within a membranous, condensed plate
of mesenchymal cells. At the initial site of ossification (ossification
centre) mesenchymal cells (osteoprogenitor cells) differentiate into
osteoblasts. The osteoblasts begin to deposit the organic bone matrix, the
osteoid. The matrix separates osteoblasts, which, from now on are located
in lacunae within the matrix. The collagen fibres of the osteoid form a woven
network without a preferred orientation, and lamellae
are not present at this stage. Because of the lack of a preferred orientation
of the collagen fibres in the matrix, this type of bone is also called woven
bone. The osteoid calcifies leading to the formation of primitive trabecular
bone.
Further deposition and calcification of osteoid at sites where compact bone is needed leads to the formation of primitive compact bone.
? Note the distinction between macroscopic and microscopic apperance when the bone is named. We again have the two macroscopically different forms of bone - trabecular bone and compact bone - but their early developmental ("primitive") forms consist of woven bone.
Through subsequent reorganisation the primitive compact and trabecular bone is converted into mature compact and trabecular bone. During reorganisation and growth, woven bone will, in time, be replaced by lamellar bone.
Intramembranous ossification does not require the existence of a cartilage bone model.
- Suitable
Slides
- sections of the developing
mandible (or some other bones of the skull) or clavicle -
H&E, van Gieson
Sections prepared to show endochondral ossification (see below) may be an
alternative if no specifically prepared slides of intramembranous ossification
are available. The periosteal collar, i.e. the manchette of bone forming
around the diaphysis of the cartilage model of the bone, is formed by a
mechanism similar to intramembranous ossfication and results in the deposition
of woven bone.
Mandible, intramembranous ossification, H&E
The developing bone will in sections usually be associated with a number of other tissues which develop in close association with it. In case of the mandible, there can be developing teeth, the tongue, skin and salivary glands.
The first job - best done at low magnification - is to find the developing
bone. It should look like a coarse meshwork (trabecular
bone) of pink tissue surrounding patches of much lighter or
unstained tissue. Lamellae are not visible (woven
bone) and the lacunae are larger than lacunae in mature bone.
Ossification centres appear as areas of a gradual transition from connective
tissue to bone. Light, pinkish bone matrix is found between the osteoblasts.
Depending on the state of development of the bone,
it is occasionally possible to find bone trabeculae which are lined by a layer
of osteoblasts. These osteblasts are depositing the first lamellae on the
already existing trabeculae. The trabeculae will therefore have a core of
woven bone, which is surrounded by lamellar bone. Compare the shapes, sizes
and frequencies of lacunae in lammellar and woven bone if both types of bone
are present.
Draw a part of trabecular bone consisting of woven bone and an ossification centre. Label the features in your drawings.

Endochondral Ossification
Most bones are formed by the transformation of cartilage "bone models", a process
called endochondral ossification. A thin sheet
of bone, the periosteal collar, is deposited
around the shaft of the cartilage model. The periosteal collar consists of
woven bone. Concurrently a periosteal bud invades
the cartilage model and allows osteoprogenitor cells to enter the cartilage.
At these sites, the cartilage is in a state of hypertrophy (very large lacunae
and chondrocytes) and partial calcification, which eventually leads to the
death of the chondrocytes.
Invading osteoprogenitor cells mature into osteoblasts, which use the framework
of calcified cartilage to deposit new bone. The bone deposited onto the cartilage
scaffold is lamellar bone. The initial site of bone deposition is called a
primary ossification centre. Secondary ossification
centres occur in the future epiphyses of the bone.
Close to the zone of ossification, the cartilage can usually be divided into a number of distinct zones :
- Reserve cartilage, furthest away from the zone of ossification, looks like immature hyaline cartilage.
- A zone of chondrocyte proliferation contains longitudinal columns of mitotically active chondrocytes, which grow in size in
- the zone of cartilage maturation and hypertrophy.
- A zone of cartilage calcification forms the border between cartilage and the zone of bone deposition.
Primary and secondary ossification centres do not merge before adulthood. Between the diaphysis and the epiphyses a thin sheet of cartilage, the epiphyseal plate, is maintained until adulthood. By continuing cartilage production, the epiphyseal plate provides the basis for growth in the length of the bone. Cartilage production gradually ceases in the epiphyseal plate as maturity is approached. The epiphyseal plate is finally removed by the continued production of bone from the diaphyseal side.
Bone formation and bone resorption go hand in hand during the growth of bone. This first deposited trabecular bone is removed (By which cells?) as the zone of ossification moves in the direction of the future epiphyses. This process creates the marrow cavity of the bones. Simultaneously, bone is removed from the endosteal surface of the compact bone forming the diaphysis and deposited on its periosteal surface which allows the bone to grow in diameter.
- Suitable Slides
- sections of bones during the early stages of their
development - H&E, van Gieson
Foetal Vertebral Column, human, H&E
Hold the section against a light background. The cartilage models will stain
very light, and the outlines of the skeletal structures they will form can
often be identified. If an ossification centre is present, it will appear
as a darker area within the cartilage model. The zonation of the cartilage
should be visible in all ossification centres. How much bone is present depends
on how far ossification has proceeded. The newly formed bone trabeculae will
often consist of lamellar bone with a more or less extensive core of darkly
staining calcified cartilage. The lamellar organisation of the bone may not
be visible.
How the ossification centre excactly will look also
depends on the plane of the section in relation to the ossification centre.
Draw the ossification centre/zone, include the adjacent
cartilage and identify the zones within it in your drawing.


- Suitable
Slides
- sections of the epiphyseal disc of growing
bones - H&E
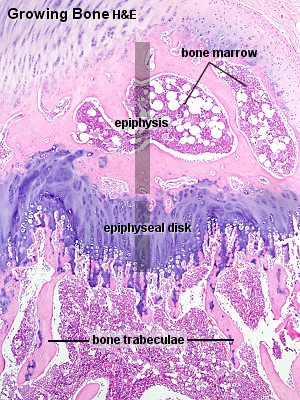
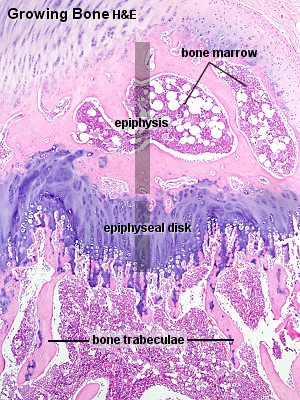 Growing Bone - H&E
Growing Bone - H&E
The cartilage model has almost entirely been transformed into bone. The only
remaining cartilage is found in the epiphyseal disk. Zones of cartilage proliferation,
hypertrophy and calcification are visible at high magnification, but only
on one side of the epiphyseal disk - towards the diaphysis, which increases
in length as the cartilage generated by the epiphyseal disc is transformed
into bone.
Osteoclasts may be found on the newly formed trabeculae or associated with
parts of the cartilage scaffold.
Draw the region of the epiphyseal disks. Identify in your
drawing the epiphyseal disk and the bone of the epiphysis and diaphysis. Indicate
the direction of cartilage proliferation in the epiphyseal disk and the direction
of bone growth.
Changes in the size and shape of bones during the period of growth imply some bone reorganisation. Osteoblast and osteoclast constantly deposit and remove bone to adjust its properties to growth-related demands on size and/or changes of tensile and compressive forces.
 Although the reorganisation of bone may not result in macroscopically visible changes of bone structure, it continues throughout life to mend damage to bone (e.g. microfractures) and to counteract the wear and tear occurring in bone. Osteoclasts and osteoblasts remain the key players in this process. Osteoclasts "drill" more or less circular tunnels within existing bone matrix. Osteoblasts deposit new lamellae of bone matrix on the walls of these tunnels resulting in the formation of a new Haversian system within the matrix of compact bone. Parts of older Haversian systems,
which may remain between the new ones, represent the interstitial lamellae in mature bone. Capillaries and nerves sprout into new Haversian canals.
Although the reorganisation of bone may not result in macroscopically visible changes of bone structure, it continues throughout life to mend damage to bone (e.g. microfractures) and to counteract the wear and tear occurring in bone. Osteoclasts and osteoblasts remain the key players in this process. Osteoclasts "drill" more or less circular tunnels within existing bone matrix. Osteoblasts deposit new lamellae of bone matrix on the walls of these tunnels resulting in the formation of a new Haversian system within the matrix of compact bone. Parts of older Haversian systems,
which may remain between the new ones, represent the interstitial lamellae in mature bone. Capillaries and nerves sprout into new Haversian canals.
Restorative activity continues in aged humans (about 2% of the Haversian systems seen in an 84 year old individual contained lamellae that had been formed within 2 weeks prior to death!). However, the Haversian systems tend to be smaller in older individuals and the canals are larger because of slower bone deposition. If these age-related changes in the appearance of the Haversian systems are pronounced they are termed osteopenia or senile osteoporosis. The reduced strength of bone affected by osteoporosis will increase the likelihood of fractures.
 Bone is, again like cartilage, surrounded by a layer of dense connective tissue, the periosteum. A thin layer of cell-rich connective tissue, the endosteum, lines the surface of the bone facing the marrow cavity. Both the periosteum and the endosteum possess osteogenic potency. Following injury, cells in these layers may differentiate into osteoblasts (bone forming cells) which become involved in the repair of the damage to the bone.
Bone is, again like cartilage, surrounded by a layer of dense connective tissue, the periosteum. A thin layer of cell-rich connective tissue, the endosteum, lines the surface of the bone facing the marrow cavity. Both the periosteum and the endosteum possess osteogenic potency. Following injury, cells in these layers may differentiate into osteoblasts (bone forming cells) which become involved in the repair of the damage to the bone.





 are
very large (up to 100 µm), multi-nucleated (about 5-10 visible in
a histological section, but up to 50 in the actual cell) bone-resorbing
cells. They arise by the fusion of monocytes (macrophage precursors in
the blood) or macrophages. Osteoclasts attach themselves to the bone matrix
and form a tight seal at the rim of the attachment site. The cell membrane
opposite the matrix has deep invaginations forming a
are
very large (up to 100 µm), multi-nucleated (about 5-10 visible in
a histological section, but up to 50 in the actual cell) bone-resorbing
cells. They arise by the fusion of monocytes (macrophage precursors in
the blood) or macrophages. Osteoclasts attach themselves to the bone matrix
and form a tight seal at the rim of the attachment site. The cell membrane
opposite the matrix has deep invaginations forming a 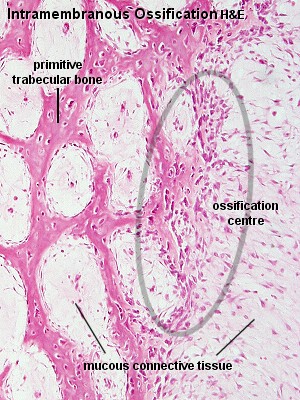



 Although the reorganisation of bone may not result in macroscopically visible changes of bone structure, it continues throughout life to mend damage to bone (e.g. microfractures) and to counteract the wear and tear occurring in bone. Osteoclasts and osteoblasts remain the key players in this process. Osteoclasts "drill" more or less circular tunnels within existing bone matrix. Osteoblasts deposit new lamellae of bone matrix on the walls of these tunnels resulting in the formation of a new Haversian system within the matrix of compact bone. Parts of older Haversian systems,
which may remain between the new ones, represent the interstitial lamellae in mature bone. Capillaries and nerves sprout into new Haversian canals.
Although the reorganisation of bone may not result in macroscopically visible changes of bone structure, it continues throughout life to mend damage to bone (e.g. microfractures) and to counteract the wear and tear occurring in bone. Osteoclasts and osteoblasts remain the key players in this process. Osteoclasts "drill" more or less circular tunnels within existing bone matrix. Osteoblasts deposit new lamellae of bone matrix on the walls of these tunnels resulting in the formation of a new Haversian system within the matrix of compact bone. Parts of older Haversian systems,
which may remain between the new ones, represent the interstitial lamellae in mature bone. Capillaries and nerves sprout into new Haversian canals.