The skin or cutis covers the entire outer surface
of the body. Structurally, the skin consists of two layers which differ in
function, histological appearance and their embryological origin. The outer
layer or epidermis is formed by an epithelium
and is of ectodermal origin. The underlying thicker layer, the dermis,
consists of connective tissue and develops from the mesoderm. Beneath the
two layers we find a subcutaneous layer of loose connective tissue or hypodermis,
which binds the skin to underlying structures. Hair, nails and sweat and sebaceous
glands are of epithelial origin and collectively called the appendages of
the skin.
The skin and its appendages together are called
the integumentary system.
The epidermis is a keratinised stratified squamous
epithelium. The main function of the epidermis is to protect the body
from harmful influences from the environment and against fluid loss. Five
structurally different layers can be identified:
- The stratum basale
is the deepest layer of the epidermis (closest to the dermis). It consists
of a single layer of columnar or cuboidal cells which rest on the basement
membrane. Basal cells are the stem cells of the epidermis. Their mitotic
activity replenishes the cells in more superficial layers as these are eventually
shed from the epidermis.
The renewal of the epidermis takes about 3 to 4
weeks in humans.
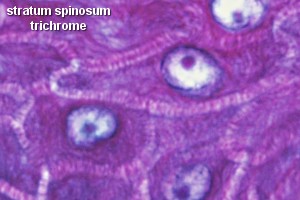
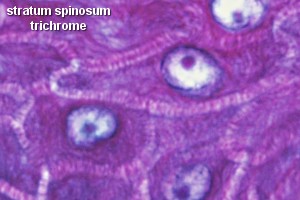 In
the stratum spinosum,
In
the stratum spinosum,
the cells become irregularly polygonal. The cells are often separated by
narrow, translucent clefts. These clefts are spanned by spine-like cytoplasmatic
extensions of the cells (hence the name of the layer and of its cells: spinous
cells), which interconnect the cells of this layer. Spines of cells
meet end-to-end or side-to-side and are attached to each other by desmosomes.
In addition to the usual organelles of cells, EM shows membrane-bound lamellar
granules in the cytoplasm of the spinous cells.
- The stratum granulosum
consists, in thick skin, of a few layers of flattened cells. Only one layer
may be visible in thin skin. The cytoplasm of the cells contains numerous
fine grains, keratohyalin granules. The keratohyalin
is not located in membrane-bound organelles but forms "free" accumulations
in the cytoplasm of the cells. The cells begin to release the contents of
the lamellar granules. The lipids contained in the granules come to fill
the entire interstitial space, which is important for the function of the
epidermis as a barrier towards the external environment.
- The stratum lucidum
consists of several layers of flattened dead cells. Nuclei already begin
to degenerate in the outer part of the stratum granulosum. In the stratum
lucidum, faint nuclear outlines are visible in only a few of the cells.
The stratum lucidum can usually not be identified in thin skin.
- In the stratum corneum,
cells are completely filled with keratin filaments (horny cells) which are
embedded in a dense matrix of proteins. Individual cells are difficult to
observe because (1) nuclei can no longer be identified, (2) the cells are
very flat and (3) the space between the cells has been filled with lipids,
which cement the cells together into a continuous membrane. In the EM, the
cell membranes appear thickened and interdigitate with those of neighbouring
cells. Closest to the surface of the epidermis, the stratum corneum has
a somewhat looser appearance. Horny cells are constantly shed from this
part of the stratum corneum.
The protection of the body by the epidermis is essentially
due to the functional features of the stratum corneum.
Variations in the thickness of the epidermis (~0.1
mm in thin skin, 1 mm or more in thick skin) are mainly the result
of variations in the thickness of the stratum corneum, although the other
layers also vary in thickness. Cells of the epidermis of the skin will at
some time of their life keratinise and are collectively also called keratinocytes.
Keratinisation should not be used as a synonym for the formation of the stratum corneum: other stratified squamous epithelia may become keratinised but may not form a stratum corneum in which cells join to form a horny cell membrane.
Other Cells of the Epidermis
The red and yellow hues of the skin are due to haemoglobin in the red blood cells, which pass through the capillaries beneath the epidermis, and carotene, which accumulates in fat cells found in the dermis and hypodermis.
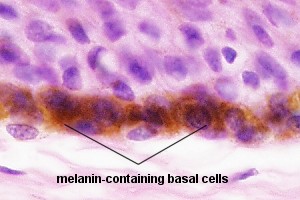
- Melanocytes
-
The brown colour component is due to melanin, which is produced in the skin itself in cells called melanocytes (typically 1000-2000 / sqr. mm). These cells are located in the epidermis and send fine processes between the other cells. In the melanocytes, the melanin is located in membrane-bound organelles called melanosomes. The cell bodies of melanocytes are difficult to distinguish in ordinary LM preparations, because the melanosomes are located mainly in the processes of the cells.
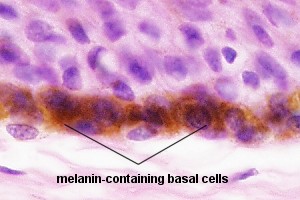 Melanocytes
can transfer melanin to keratinocytes - mainly to the basal cells. The
fine processes of melanocytes may invade keratinocytes and bud-off part
of the melanocyte-cytoplasm, including the melanosomes, within the keratinocytes.
Melanin protects the chromosomes of mitotically active basal cells against
light-induced damage.
Melanocytes
can transfer melanin to keratinocytes - mainly to the basal cells. The
fine processes of melanocytes may invade keratinocytes and bud-off part
of the melanocyte-cytoplasm, including the melanosomes, within the keratinocytes.
Melanin protects the chromosomes of mitotically active basal cells against
light-induced damage.
Pigmentation is not just under the control of light. Hormones produced by the pituitary and the adrenal glands also affect pigmentation. Diseases of these two endocrine organs often result in changes of pigmentation of the skin.
Although melanocytes are also ectodermal in origin, they are derived exclusively from the neural crest of the embryo, from where they migrate to all other parts of the body.
- Langerhans Cells
-
are another cell type found within the epidermis. Morphologically they are not unlike melanocytes, but functionally they are more closely related to macrophages. They are important in immune reactions of the epidermis. Their fine processes form a network between the cells of the epidermis and phagocytose antigens which have entered the epidermis. Langerhans cells may only be temporary residents of the skin. If they have come into contact with an antigen, they can migrate to regional lymph nodes, where they initiate an immune response.
- T-lymphocytes
-
are, like Langerhans cells, a group of cells functioning
in the immune system. Some of them will be present in the epidermis. Together
with Langerhans cells they are sometimes referred to asSALT,
i.e. skin-associated
lymphoid tissue.
The dermis is the thick layer of connective tissue to which the epidermis is attached. Its deepest part continues into the subcutaneous tissue without a sharply defined boundary. Its thickness is for this reason difficult to determine but 1-2 mm is a good guestimate for "average" skin. The dermis may be divided into two sublayers (again without a sharp boundary):
Elastic fibres are found in both the papillary (fine fibres) and reticular (coarse fibres) layers.
They can not be identified in H&E stained sections.
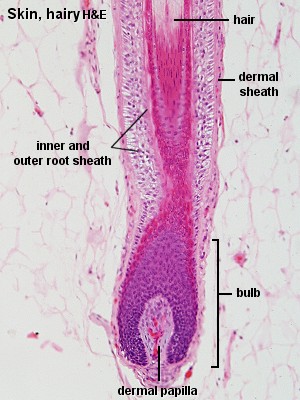
Hair
A characteristic feature of the human skin is the apparent lack of hair (pili)
on most of the body surface. This is actually not quite true. Most of the
skin is haired although the hair in most areas is short, fine and only lightly
pigmented. This type of hair is called vellus hair.
Truly hairless are only the palms of hands and soles of feet, the distal
phalanges and sides of fingers and toes and parts of the external genitalia.
In those parts of the skin which we perceive as "hairy" we find terminal hairs. The free part of each hair is called the shaft. The root of each hair is anchored in a tubular invagination of the epidermis, the hair follicle, which extends down into the dermis and, usually, a short distance into the hypodermis. The deepest end of the hair follicle forms an enlargement, the bulb. Cells in the bulb are mitotically active. Their progeny differentiates into the cell types which form the hair and the cells that surround its root, the root sheath. Hair cells keratinise within the lower one-third of the hair follicle. Above this level it is not possible to identify individual cells within the hair. Each hair follicle has an associated bundle of smooth muscle, the arrector pili muscle. This muscle inserts with one end to the papillary layer of the dermis and with the other end to the dermal sheath of the hair follicle.
Hair growth is discontinuous. Hairs are lost and replaced by new ones. The hair follicle goes through different stages that reflect the discontinuous hair growth. Anagen is the phase of growth. The resting stage is called telogen. The length of the anagen is variable in different regions of the body - lasting only a few months for hair of the eyebrows and eyelashes but 2 to 5 years for hair of the scalp. Hair growth is controlled by a number of hormonal and hereditary factors and their interactions.
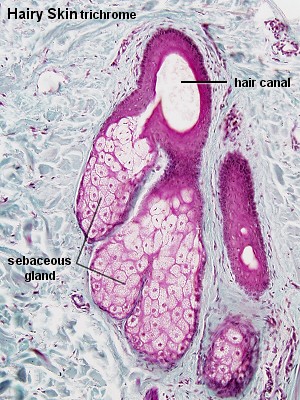
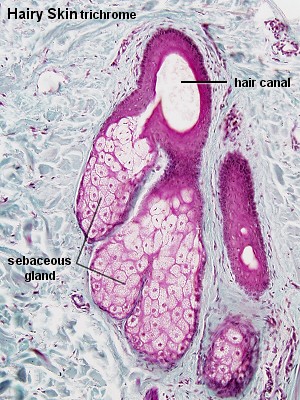
Sebaceous Glands
Sebaceous glands empty their secretory product into the upper parts of the
hair follicles. They are therefore found in parts of the skin where hair is
present. The hair follicle and its associated sebaceous gland form a pilosebaceous
unit.
Sebaceous glands are also found in some of the areas where no hair is present,
for example, lips, oral surfaces of the cheeks and external genitalia.
Sebaceous glands are as a rule simple and branched (Remember
the nomenclature of glands!). The secretory
portion consists of alveoli. Basal cells in the outermost layer of
the alveolus are flattened. Basal cells are mitotically active. Some of the
new cells will replenish the pool of basal cells, while the remaining cells
are displaced towards the centre of the alveolus as more cells are generated
by the basal cells. The secretory cells will gradullay accumulate lipids and
grow in size. Finally their nuclei disintegrate, and the cells rupture. The
resulting secretory product of lipids and the constituents of the disintegrating
cell is a holocrine secretion.
The lipid secretion of the sebaceous glands has no softening effect on the
skin, and it has only very limited antibacterial and antifungoid activity.
Its importance in humans is unclear. Clinically the sebaceous glands are important
in that they are liable to infections (e.g. with the
development of acne).
- Suitable Slides
- slides of hairy skin
or thin skin - H&E, trichrome,
van Gieson
Skin, hairy - trichrome, H&E
Sebaceous glands will be present in all types of
skin other than thick skin. Their numbers should correlate with the number
of hair follicles. If your section does not contain hair follicles you are
unlikely to see a good sebaceous gland. Sebaceous glands are usually
embedded in the dermis. Although they empty into the hair canal of the hair
follicle, this point will only be visible for a few of them because of the
thinness of the sections. It should however be possible to follow the fate
of the secretory cells. Deep in the sebaceous glands cells are smaller with
intact nuclei. Cell size increases with the accumulation of sebum as the
cells are gradually displaced towards the opening of the gland into the
hair follicle. The nuclei condense, become darker and irregularly shaped.
Draw a sebaceous gland. Emphasise the appearance of the
secretory cells in different parts of the gland. If possible include part
of the associated hair follicle.

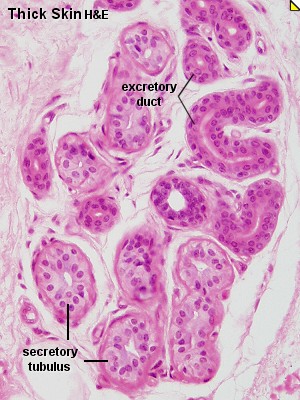
Sweat Glands
Two types of sweat glands are present in humans. They are distinguished by
their secretory mechanism into merocrine (~eccrine)
sweat glands and apocrine sweat glands.
In addition, they differ in their detailed histological appearance and in
the composition of the sweat they secrete.
Merocrine sweat glands are the only glands of
the skin with a clearly defined biological function. They are of critical
importance for the regulation of body temperature. The skin contains ~3,000,000
sweat gland which are found all over the body - with
the exception of, once again, parts of the external genitalia.
- Sweat glands are simple tubular glands.
The secretory tubulus and the initial part of the excretory duct are coiled
into a roughly spherical ball at the border between the dermis and hypodermis.
- The secretory epithelium is cuboidal or low columnar. Two types of cells may be distinguished: a light type, which secretes the watery eccrine sweat, and a dark type, which may produce a mucin-like secretion. The cells have slightly different shapes and, as a result of the different shapes, the epithelium may appear pseudostratified.
- A layer of myoepithelial cells is found between
the secretory cells of the epithelium and the basement membrane.
- The excretory duct has a stratified cuboidal epithelium (two layers of cells).
The excretory ducts of merocrine sweat glands empty
directly onto the surface of the skin.
Apocrine sweat glands occur in, for example, the axilla. They are stimulated by sexual hormones and are not fully developed or functional before puberty. Apocrine sweat is a milky, proteinaceous and odourless secretion. The odour is a result of bacterial decomposition and is, at least in mammals other than humans, of importance for sexual attraction.
The histological structure of apocrine sweat glands is similar to that of
merocrine sweat glands, but the lumen of the secretory tubulus is much larger
and the secretory epithelium consists of only one major cell type, which looks
cuboidal or low columnar. Apocrine sweat glands as such are also much larger
than merocrine sweat glands.
The excretory duct of apocrine sweat glands does not
open directly onto the surface of the skin. Instead, the
excretory duct empties the sweat into the upper part of the hair follicle.
Apocrine sweat glands are therefore part of the pilosebaceous unit.
Some texts argue that the apocrine sweat glands use
a merocrine or a combined merocrine / apocrine secretory mechanism.


 In
the
In
the 

 Melanocytes
can transfer melanin to keratinocytes - mainly to the basal cells. The
fine processes of melanocytes may invade keratinocytes and bud-off part
of the melanocyte-cytoplasm, including the melanosomes, within the keratinocytes.
Melanin protects the chromosomes of mitotically active basal cells against
light-induced damage.
Melanocytes
can transfer melanin to keratinocytes - mainly to the basal cells. The
fine processes of melanocytes may invade keratinocytes and bud-off part
of the melanocyte-cytoplasm, including the melanosomes, within the keratinocytes.
Melanin protects the chromosomes of mitotically active basal cells against
light-induced damage.




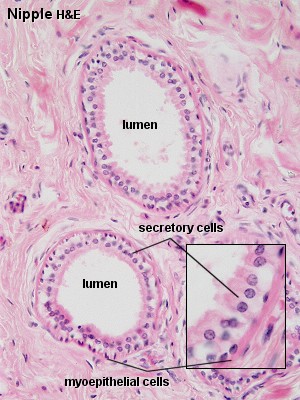 Nipple
- H&E
Nipple
- H&E