EPITHELIA
Epithelia are tissues consisting of closely apposed cells without intervening intercellular substances. Epithelia are avascular, but all epithelia "grow" on an underlying layer of vascular connective tissue. The connective tissue and the epithelium are separated by a basement membrane. Epithelium covers all free surfaces of the body. Epithelium also lines the large internal body cavities, where it is termed mesothelium. Furthermore, the internal surfaces of blood and lymph vessels are lined by epithelium, here called endothelium.
Epithelia are classified on the basis of the number of cell layers and the shape of the cells in the surface layer.
- If there is only one layer of cells in the epithelium, it is designated simple.
- If there are two or more layers of cells, it is termed stratified.
- Cells in the surface layer are, as a rule, described according to their height as squamous (scale- or plate-like), cuboidal or columnar.
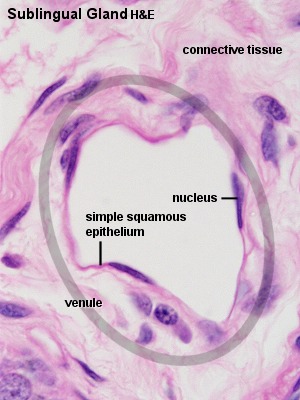
- Simple squamous epithelium
-
This type is composed of a single layer of flattened, scale- or plate-like cells. It is quite common in the body. The large body cavities and heart, blood vessels and lymph vessels are typically lined by a simple squamous epithelium. The nuclei of the epithelial cells are often flattened or ovoid, i.e. egg-shaped, and they are located close to the centre of the cells.
- Simple cuboidal epithelium
-
Cells appear cuboidal in sections perpendicular to the surface of the epithelium. Viewed from the surface of the epithelium they look rather like small polygons. Simple cuboidal epithelium occurs in small excretory ducts of many glands, the follicles of the thyroid gland, the tubules of the kidney and on the surface of the ovaries.
Can there be "low cuboidal" epithelia?
- Simple columnar epithelium
-
The cells forming a simple columnar epithelium are taller than they are wide. The nuclei of cells within the epithelium are usually located at the same height within the cell - often close to the base of the cell. An example is the simple columnar epithelium which lines the internal surface of the gastrointestinal tract (GIT) from the cardia of the stomach to the rectum.
 |
? Identifying Epithelia
The outlines of individual epithelial cells are not always visible, and it may be difficult to identify the shape of the cells. It is often helpful to look at the shape, location and spacing of the nuclei in the epithelium, which together will allow a very good guess at the shape of the cells forming the epithelium. |
 |
How many cell layers are visible in a section depends very much on the angle between the section plane and the surface of the epithelium. Oblique sections of epithelium will be visible in almost all slides of organs in which epithelium lines a surface with a very irregular profile. A single surface is usually not lined by several types of epithelia. The number of epithelial cell layers will usually be the smallest number of layers visible anywhere along the surface lined by the epithelium. |
- Suitable Slides
- simple squamous epithelium: any section containing blood vessels or sections of organs which include the serosa of the organs - H&E
simple cuboidal epithelium: sections of ovaries, thyroid gland, kidney or large glands (e.g. parotid gland) with well preserved small ducts
simple columnar epithelium: sections of the small intestine (duodenum, jejunum or ileum), uterus (uterine glands), liver (large bile ducts) or gall bladder - H&E, trichrome
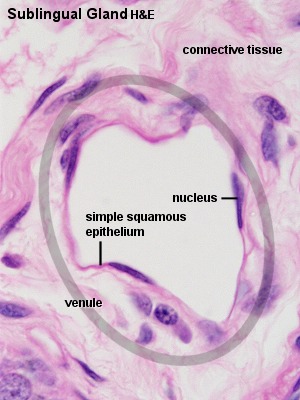 Sublingual Gland, human, H&E
Sublingual Gland, human, H&E
Blood vessels are probably present in all sections you will ever see. With very few exceptions, they are lined by a simple squamous epithelium. The individual epithelial cells are extremely fattened and form a much larger part of the surface than individual cuboidal or columnar cells. The nuclei of the epithelial cells are also flattened. Not every epithelial cell nucleus will be included in the plane of the section, and if the vessel is very small (e.g. a capillary), there may be no visible nuclei in the epithelial lining. Capillaries and other small vessels are easily deformed during tissue processing and the epithelium of larger vessels may be damaged or look
corrugated. It may therefore take a little more patience than you expect to find a "good" simple squamous epithelium.
Draw a small vessel with its epithelial lining, label the features visible in your drawing and include a suitable scale.
 Duodenum, rat, H&E and Ileum, human - H&E
Duodenum, rat, H&E and Ileum, human - H&E
The small intestines are lined by a simple cuboidal epithelium. Most of the epithelial cells (enterocytes) are involved in the absorption of components of the digested food in the lumen of the intestines. Complex folds of the intestinal lining increase the surface area available for absorption. The sections plane will therefore often pass at an oblique angle through the epithelium. The epithelium may look stratified where this happens. Scan along the epithelium until you find a spot where it is cut perpendicular to its surface, i.e. where it looks like a simple columnar epithelium. Mucus producing goblet cells
are a second cell type of this epithelium. Mucus stains only weakly or not at all in H&E stained sections. Round, light "hollows" in the epithelium represent the apical cytoplasm of the goblet cells, which is filled with mucin-containing secretory vesicles.
Microvilli extend from the apical surface of epithelial cells into the intestinal lumen. They increase surface area by a factor of ~20 and thereby facilitate absorption. Together, the microvilli are visible as a light red band along the upper limit of the epithelium - the brushborder.
Draw and label the epithelium. Include goblet cells in your drawing.
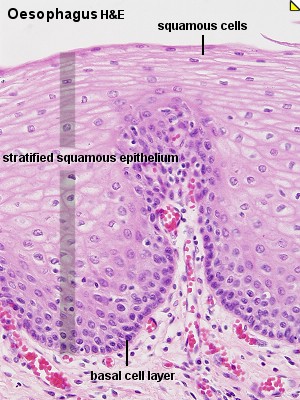
- Stratified squamous epithelium
-
Stratified squamous epithelia vary in thickness depending on the number of cell layers present. The deepest cells, which are in contact with the basement membrane, are cuboidal or columnar in shape. This layer is usually named the basal cell layer, and the cells are called basal cells. Basal cells are mitotically active and replace the cells of the epithelium which are lost by "wear and tear". The basal cell layer is followed by layers of cells with polyhedral outlines. Close to the surface of the epithelium, cells become more flattened. At the surface of the epithelium, cells appear like flat scales -
similar to the epithelial cells of simple squamous epithelia.
Remember that it is the shape of the cell which form the surface of the epithelium which gives the name to the epithelium!
- Stratified cuboidal and columnar epithelia
-
are not common. A two-layered cuboidal epithelium is, for example, seen in the ducts of the sweat glands. Stratified columnar epithelia are found in the excretory ducts of the mammary gland and the main excretory duct of the large salivary glands.
- Suitable Slides
- stratified squamous epithelium: sections of the oesophagus or tongue - H&E, van Gieson
stratified cuboidal epithelium: skin (excretory ducts of sweat glands) - H&E
stratified columnar epithelium: sections of the parotid gland or mammary gland - H&E
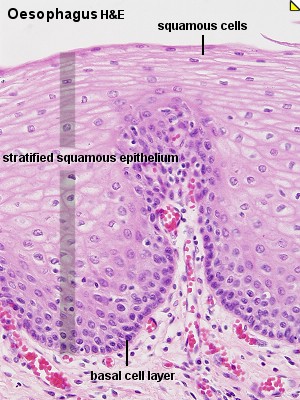 Oesophagus, human - H&E
Oesophagus, human - H&E
The oesophagus is lined by a stratified squamous epithelium consisting of many cell layers. Basal cells often form a well defined layer at the border of the epithelium to the underlying connective tissue. The underlying connective tissue forms finger-like extensions towards the lumen of the oesophagus, which are called papillae. The border between epithelium and connective tissue may appear quite irregular because of the papillae. This irregular border aids in anchoring of the epithelium to the connective tissue. If these extensions are not cut exactly along their long axis, they may look like isolated small islands of connective tissue and
blood vessels within the epithelium.
Draw the stratified squamous epithelium of the oesophagus and label your drawing. Try to draw a little schematic illustration which shows how the plane of section would effect the appearance of the connective tissue extensions.
Parotid Gland, human - H&E
Stratified columnar epithelia are found in the largest excretory ducts of some glands. The parotid gland, a large salivary gland, is one of them. Several epithelial types are found in the duct system of the parotid. The smallest ducts, which are embedded in the secretory tissue (intralobular ducts), are lined by cuboidal or columnar epithelia. Small ducts, which are embedded in connective tissue located between areas of secretory tissue (interlobular ducts), are lined by columnar or pseudostratified epithelia. These ducts finally coalesce to form the main excretory duct of the parotid which is lined by a stratified columnar epithelium.
Draw the stratified columnar epithelium seen in the largest ducts and label your drawing.


Pseudostratified and Transitional Epithelia
These two types of epithelia are difficult to classify using the shape of the cells in the surface layer and the number of the cell layers as criteria.
- Transitional epithelium
-
The shape of the cells varies with the degree of distension of the organ in the epithelium which lines the excretory passages of the urinary system - transitional epithelium. In the "relaxed" state of the epithelium, it seems to be formed by many cell layers. The most basal cells have a cuboidal or columnar shape. There are several layers of polyhedral cells, and, finally, a layer of superficial cells, which have a convex, dome-shaped luminal surface. In the distended state of the epithelium only one or two layers of cuboidal cells are followed by a superficial layer of large, low cuboidal or squamous cells. In the distended state the epithelium will resemble a
stratified squamous epithelium.
Transitional epithelium is found exclusively in the excretory urinary passages (the renal calyces and pelvis, the ureter, the urinary bladder, and part of the urethra).
- Pseudostratified columnar epithelium
-
 All cells of this type of epithelium are in contact with the basement membrane, but not all of them reach the surface of the epithelium. Nuclei of the epithelial cells are typically located in the widest part of the cell. Consequently, the nuclei of cells which do or do not reach the surface of the epithelium are often located at different heights within the epithelium and give the epithelium a stratified appearance. The epithelium will look stratified but it is not - hence its name "pseudostratified". Pseudostratified
columnar epithelia are found in the excretory ducts of many glands.
All cells of this type of epithelium are in contact with the basement membrane, but not all of them reach the surface of the epithelium. Nuclei of the epithelial cells are typically located in the widest part of the cell. Consequently, the nuclei of cells which do or do not reach the surface of the epithelium are often located at different heights within the epithelium and give the epithelium a stratified appearance. The epithelium will look stratified but it is not - hence its name "pseudostratified". Pseudostratified
columnar epithelia are found in the excretory ducts of many glands.
- Suitable Slides
- transitional epithelium: sections of ureter or urinary bladder - H&E
pseudostratified epithelium: sections of the trachea - H&E
 Ureter, monkey - H&E
Ureter, monkey - H&E
At a first glance a transitional epithelium looks like a stratified cuboidal epithelium. Several layers of nuclei appear to be topped by a layer of dome-shaped cells which bulge into the lumen of the ureter. The shape of the surface cells and the number of layers change if the ureter is distended. The number of layers decreases. This decrease should tell us that many of the nuclei located in different layers of the epithelium belong to cells which are all in contact with the basement membrane. With distension, the shape of the cells in the surface layer will become squamous.
Draw the epithelium and label the features you can see. Add a simple schematic drawing of how you expect the epithelium to look like if the ureter is distended.
It has not yet been resolved if all the epithelial cells are in contact with the basement membrane. Some texts consider transitional epithelium as a specialised stratified epithelium while others group it with pseudostratified epithelia. Maybe it is best to also consider it "transitional" in this regard.
 Trachea, human - H&E
Trachea, human - H&E
At least two, sometimes three layers of nuclei are seen in the pseudostratified columnar epithelium lining the trachea. The nuclei belong to cells which are all in contact with the basement membrane. The epithelial lining of the trachea is also one of the few examples of a basement membrane visible in H&E stained sections. Epithelial cells can be ciliated or they can be goblet cells (unicellular exocrine glands). Capillaries and small vessels are visible in the connective tissue beneath the epithelium.
A ciliated pseudostratified columnar epithelium with goblet cells is a characteristic feature of parts of the respiratory system, where it is call respiratory epithelium. It contains several cell types in addition to ciliated cells and goblet cells.
Draw the epithelium at high magnification and label your drawing.
Special Cytological Features of Epithelia
Basement membrane
Epithelia are separated from the underlying connective tissue by an extracellular supporting layer called the basement membrane. The basement membrane is composed of two sublayers. The basal lamina (about 100 nm thick) consists of fine protein filaments embedded in an amorphous matrix. It is produced by the epithelial cells. The reticular lamina consists of reticular fibres embedded in ground substance. The components of the reticular lamina are synthesised by cells of the connective tissue underlying the epithelium. In addition to its function as support of the epithelium, the
basal lamina acts as a selectively permeable filter between epithelium and connective tissue.
Unless special stains are used, the basement membrane is rarely visible using light microscopy. You can read more about reticular fibres and ground substance on the "Connective Tissues" page.
Specialisations of the apical surface
Microvilli and stereocilia are finger- or thread-shaped extensions of the epithlial cells. Their main function is to increase the surface area of epithelial cells. They are typically found in epithelia active in absorption. Microvilli contain actin filaments, which are in contact with the terminal web of the cell . The only difference between microvilli and stereocilia is their length. Microvilli are much shorter than stereocilia. Stereocilia are, despite their name ("cilia"), not actively moving structures.
. The only difference between microvilli and stereocilia is their length. Microvilli are much shorter than stereocilia. Stereocilia are, despite their name ("cilia"), not actively moving structures.
Using light microscopy, stereocilia are difficult to discern from cilia.
Specialisations of the lateral and basal surfaces
Connective tissue is responsible for the structural integrity of most organs. As mentioned above, it is absent from epithelia and cell-to-cell contact, and tissue integrity has to be taken care of by the epithelial cells. Several specialisations in the lateral and basal parts of the cell membranes of the epithelial cells mediate these functions.
- Desmosomes
-
are specialisations of the lateral cell membranes which mediate cell adhesion. Proteins inserted into the cell membrane of the adjacent cells form a protein-"zipper" linking the cells. Fibers of the cytoskeleton attach to the cytoplasmic side of the desmosome to stabilise the area of contact. Hemi-desmosomes mediate the attachment of the epithelial cells to the basement membrane.
A group of glycoproteins (cadherins) inserted into the opposing plasma membranes mediate cell-to-cell adhesion at desmosomes and also at the adhesion zones or patches mentioned below. Integrins, another group of proteins, allow the cell to attach to the matrix proteins of the basement membrane.
- A zone of adhesion (zonula adherens)
-
is structurally not as well-characterised as the desmosomes. The zonula adherens typically appears as a close and consistent apposition (15-20 nm) of the cell membranes close to the apical cell surface and surrounding the entire cell. Again, fibres of the cytoskeleton insert into the cytoplasmic side of this membrane specialisation.
- Additional patches of adhesion (maculae adherentes),
-
which structurally resemble the zonula adherens, are found scattered over the lateral surfaces of the epithelial cell.
- The above mentioned membrane specialisations mediate cell-adhesion but are less well suited to support one of the essential functions of epithelia - the isolation of the interior of the body from the outside world. A tight junction (zonula occludens) between epithelial cells mediates this aspect of epithelial function.
-
Proteins inserted into the cell membranes of adjacent cells "stitch" the membranes of the cells together and provide an effective barrier to the diffusion of substances from the outside of the epithelium (called luminal side if the epithelium covers the surface of a tubular structure). Several "rows of stitches" may be found. Their number depends on the demand to reduce diffusion across the epithelium. Each of these rows reduces diffusion by about a factor 10 of what it was "before".
are cells or aggregations of cells whose function is secretion.
- Exocrine glands release the secretory product via a system of ducts that opens upon one of the surfaces of the body which are in contact with the external world (skin, gastro-intestinal tract etc.).
- Endocrine glands release their secretory product (typically hormones) into the spaces between the secretory cells (extracellular space) from which it enters the bloodstream.
Both endocrine and exocrine glands are developmentally derived from epithelia, which form a down-growth into the underlying connective tissue. The cells forming this down-growth then develop the special characteristics of the mature gland. Exocrine glands maintain the connection with the body surface whereas it is lost by endocrine glands.
Classification of Exocrine Glands
Exocrine glands may be classified according to cell number, and/or the shape and branching pattern of their secretory portions and ducts.
- Unicellular Glands
-
consist of a single secretory cell. In mammals the only example of unicellular
exocrine glands are goblet cells, which occur in the epithelium of many
mucous membranes. Goblet cells secrete the glycoprotein mucin, which by
the uptake of water is converted into a slimy substance, mucus.
- Multicellular glands
-
 The
simplest form of a multicellular gland is a secretory
epithelial sheath - a surface epithelium consisting entirely of
secretory cells (e.g. the epithelium lining the
inner surface of the stomach, where the mucous secretion protects the
stomach wall from the acidic contents of the stomach). Other multicellular
glands have their secretory portion embedded in the connective tissue
underlying the epithelium. The secretion is either discharged directly
from the secretory portion onto the epithelium or reaches the epithelium
via a duct system that consists of non-secretory cells.
The
simplest form of a multicellular gland is a secretory
epithelial sheath - a surface epithelium consisting entirely of
secretory cells (e.g. the epithelium lining the
inner surface of the stomach, where the mucous secretion protects the
stomach wall from the acidic contents of the stomach). Other multicellular
glands have their secretory portion embedded in the connective tissue
underlying the epithelium. The secretion is either discharged directly
from the secretory portion onto the epithelium or reaches the epithelium
via a duct system that consists of non-secretory cells.
|
The secretory portion may have a variety of shapes. Secretory cells
may form
- tubes in tubular
glands,
- acini in acinar
glands or
- alveoli in alveolar
glands.
|
 |
Combinations exist - the pancreas is a tubulo-acinar gland, in which each section of the secretory system has a specialized function.
The precursors of digestive enzymes are produced by the acinar cells. Tubular cells secrete the alkaline bicarbonate solution which eventually neutralizes the acidic contents of the stomach that are released into the duodenum.
Multicellular glands with an unbranched excretory duct are called simple. We talk about a compound gland when the excretory duct is branched. Finally, the part of the gland consisting of secretory cells is branched in a (surprise!) branched gland.
The classification scheme may appear somewhat elaborate - but there are many exocrine glands around. All of them can be identified and described by this scheme, and some ideas about their function can be derived from this description.
- Suitable Slides
- unicellular exocrine glands (goblet cells): sections of intestines (duodenum, jejunum, ileum or colon) or trachea - H&E
secretory epithelial sheath: stomach - H&E
straight tubular glands: sections of stomach (principal glands) or colon (intestinal glands) - van Gieson, H&E
coiled tubular glands: sections of skin (sweat glands) - see lab section on the Integumentary System page.
 Colon, human - van Gieson
Colon, human - van Gieson
Straight tubular glands extend from the surface of the colon into the underlying connective tissue. Although they are present throughout the intestines they are largest in the colon and, because of the smooth inner surface of the colon, they often show in good longitudinal or transverse sections. The lumen of the glands is narrow and surrounded by secretory cells of several types, which include goblet cells. The connective tissue beneath the epithelium and surrounding the glands in the colon contains more cells than the connective tissue beneath other epithelia that were considered on this page. This is a characteristic feature of the epithelia in the digestive
system.Glands cut at slightly oblique angles will connect to the lumen outside of the plane of the section.
If possible, draw both longitudinally and transversely sections intestinal glands. Include part of the surrounding connective tissue and surface epithelium.
Exercise: Draw a compound branched tubulo-acinar gland. Indicate in your drawing which parts are secretory and which parts are non-secretory.
The secretory cells can release their secretory products by one of three mechanisms.
 |
- Merocrine secretion corresponds to the process of exocytosis. Vesicles open onto the surface of the cell, and the secretory product is discharged from the cell without any further loss of cell substance.
|
 |
- Apocrine secretion designates a mechanism in which part of the apical cytoplasm of the cells is lost together with the secretory product. The continuity of the plasma membrane is restored by the fusion of the broken edges of the membrane, and the cell is able to accumulate the secretory product anew. This mechanism is used by apocrine sweat glands, the mammary glands and the prostate.
|
 |
- Holocrine secretion designates the breakdown and discharge of the entire secretory cell. It is only seen in the sebaceous glands of the skin.
|
There are two additional mechanisms by which secretory cells can release their products. Lipid soluble substances may diffuse out of the secretory cell (e.g. steroid hormone producing endocrine cells). Transporters (membrane proteins) may actively move the secretory product across the plasma membrane (e.g. the acid producing parietal cells of the gastric glands). These secretory mechanisms may not involve any light microscopically visible specialisations of the cell.
The relationship between the secretory tissue (parenchyma) of glands and the supporting connective tissue is similar in most larger glands. Externally the entire gland is surrounded by a layer of dense connective tissue, the capsule. Connective tissue sheets (septae) extend from the capsule into the secretory tissue and subdivide the gland into a number of lobes. Thinner connective tissue septae subdivide the lobes into a number of lobules. Reticular connective tissue (hardly visible in H&E
stained sections) surrounds and supports the secretory units of the glands (alveoli, acini etc.) and the initial parts of the excretory ducts if present.
Blood and lymph vessels as well as nerves penetrate the capsule and form a delicate network between the secretory units and the initial parts of the duct system.
The main excretory duct conveys the secretory product to one of the external surfaces of the body. Other parts of the duct system are named according to their relation to the lobes and lobules of the gland.
- Lobar ducts are are large branches of the main duct which extend to the lobes of the gland. They may be called
- Interlobar ducts if they are found in the connective tissue surrounding the lobes. Interlobar ducts branch and give rise to
- Interlobular ducts, which are found in the connective tissue surrounding the individual lobules of the gland. Branches of the interlobular ducts enter the lobules and are now called
- Intralobular ducts. The terminal branches of the duct system, which connect intralobular ducts with the secretory units of the gland, are called
- Intercalated ducts.
The appearance of the different portions of the duct system is quite variable from gland to gland and may allow the identification of the gland. Quite often, the appearance of parts of the duct system also permits some deductions about their functions.
? Note that lobes and lobules are defined by their relationship to each other. Many small lobules may form one large lobe. Neither size nor the spatial relationship between different parts of the tissue can be unequivocally determined in a single, two-dimensional section of the tissue. Lobes and interlobar ducts may therefore be difficult to distinguish from lobules and interlobular ducts.
- Suitable Slides
- alveolar gland: lactating mammary gland - see lab section on the Female Reproductive System page.
serous and mucous acinar glands: sections of parotid gland, sublingual gland or tongue (lingual salivary glands) - H&E
 Parotid Gland, human - H&E
Parotid Gland, human - H&E
Find an area of secretory tissue at low magnification, and scan over this area at high magnification. Within the lobules and between the acini of the parotid you can find two types of ducts. Since they are both located within the lobules they are both intralobular ducts. Striated ducts are lined by a simple tall columnar epithelium. Intercalated ducts are lined by a simple cuboidal epithelium and connect individual acini to the striated ducts.
Try to capture the features of the acini, intercalated and striated ducts in one compound drawing which shows how they connect to each other. Label your drawing.
Parotid Gland, human and Sublingual Gland, human - H&E
Many secretory cells and the secretory structures formed by them belong to
one of two morphologically distinct forms: they can be serous
or mucous. Serous secretions have a low viscosity,
i.e. they are rather "watery". Mucous secretions have a high viscosity, i.e.
they are rather "slimy". The apical cytoplasm of the cells forming serous
acini is usually well-stained. Secretory vesicles are visible in the
apical cytoplasm in well-preserve tissue. The nuclei are round or slightly
ovoid and located in the basal cytoplasm of the cells. The
bluish color of the basal cytoplasm reflects the presence of large amounts
of rough endoplasmatic reticulum.
The contents of the secretory vesicles in the apical cytoplasm of cells forming mucous acini are only weakly stained. These empty-looking vesicles give the apical cytoplasm of mucus-producing cells a distinct "foamy" or "frothy" appearance. The nuclei of mucous cells appear darker and smaller than the nuclei of serous cells. They also seem to be "pressed" against the basal limit of the cells and may look flattened with an angular ("edgy") outline. Glands containing mucous acini (e.g. the sublingual glands) are called mucous glands. Glands containing serous acini (e.g. the parotid
glands) are called serous glands. If both types of acini are present the gland is muco-serous.
Identify and draw serous and mucous acini at high magnification. Label your drawing. Make sure that the features which characterise serous and mucous acini are visible in your drawing - if necessary use a little artistic freedom.