- is a specialised type of connective tissue.
- consists, like other connective tissues, of cells and extracellular components.
- does, unlike other connective tissues, not contain vessels or nerves.
- is surrounded by a layer of dense connective tissue, the perichondrium.
Cartilage is rather rare in the adult humans, but it is very important during
development because of its firmness and its ability to grow rapidly. In developing
humans, most of the bones of the skeleton are preceded by a temporary cartilage
"model". Cartilage is also formed very early during the repair of bone fractures.
Types of Cartilage
Hyaline cartilage develops, like other types of connective tissue, from mesenchymal
cells. From about the fifth foetal week precursor cells become rounded and
form densely packed cellular masses, centres
of chondrification. The cartilage-forming cells, chondroblasts,
begin to secrete the components of the extracellular matrix of cartilage.The
extracellular matrix consists of, ground substance (hyaluronan, chondroitin
sulfates and keratan sulfate) and tropocollagen, which polymerises extracellularly
into fine collagen fibres.
Collagen type II is the dominant form in almost all types of cartilage.
As the amount of matrix increases the chondroblasts become separated from each
other and are, from this time on, located isolated in small cavities within
the matrix, the lacunae. Concurrently the cells
differentiate into mature cartilage cells, chondrocytes .
.
Growth occurs by two mechanisms
- Interstitial growth - Chondroblasts within the existing cartilage divide and form small groups of cells, isogenous groups, which produce matrix to become separated from each other by a thin partition of matrix. Interstitial growth occurs mainly in immature cartilage.
- Appositional growth - Mesenchymal cells
surrounding the cartilage in the deep part of the perichondrium (or the
chondrogenic layer) differentiate into chondroblasts. Appositional growth
occurs also in mature cartilage.
Like all protein-producing cells, chondroblasts contain plenty of rough endoplasmatic
reticulum while they produce matrix. The amount of rough endoplasmatic reticulum
decreases as the chondroblasts mature into chondrocytes. Chondrocytes fill
out the lacunae in the living cartilage.
The matrix appears structureless because the
collagen fibres are too fine to be resolved by light microscopy (~20nm),
and because they have about the same refractive index as the ground substance.
Collagen accounts for ~ 40% of the dry weight of the matrix.
The matrix near the isogenous groups of chondrocytes contains larger amounts
and different types of glycosaminoglycans than the matrix further away from
the isogenous groups. This part of the matrix is also termed territorial
matrix or capsule. In H&E stained sections the territorial matrix
is more basophilic, i.e. it stains darker. The remainder of the matrix is
called the interterritorial matrix. Fresh cartilage
contains about 75% water which forms a gel with the components of the ground
substance. Cartilage is nourished by diffusion of gases and nutrients through
this gel.
- Suitable Slides
- sections of the trachea
or larynx - H&E, van
Gieson
Trachea, cat, H&E and Trachea,
cat, van Gieson
Both stains are equally well suited to look at the organisation of hyaline
cartilage. The van Gieson method stains collagen red. The cartilage appears
as a wide red zone underneath the epithelium and loose connective tissue,
which line the lumen of the trachea. The staining may appear a little lighter
close to the lacunae. This lighter stained zone defines the territorial matrix
surrounding the lacunae and chondrocytes. Colour intensities appear reversed
in the H&E stained section. The two compartments of the matrix are usually
better defined than in van Gieson stained sections. The interterritorial matrix
appears very light; the territorial matrix is somewhat darker. Groups of chondrocytes
surrounded by these lighter (van Gieson) or darker (H&E) staining zones
belong to the same isogenous group. A layer of dense connective tissue surrounding
the cartilage and blending with it is the perichondrium.
The isogenous groups may form small "squares" (e.g. four chondrocytes, separated
by thin cartilage membranes, in a 2x2 arrangement) or short columns (e.g.
four chondrocytes in a 1x4 arrangement).
Draw a small section of the cartilage and identify in your
drawing territorial matrix, interterritorial matrix, isogenous groups, and
chondrocytes. Think about how the spatial arrangement of chondrocytes in the
isogenous group may reflect patterns of cell divisions.


- Suitable Slides
- Sections of the epiglottis
- elastin
Epiglottis, human, elastin
Preparations of the epiglottis are usually dominated by the cartilage surrounded
by varying amounts of connective tissue and epithelia. The appearance of the
cartilage (in this preparation a blue-green colour) will depend on the method
used to show tissue components other than elastic fibres. Although the matrix
appears blue-green, the typical organisation of cartilage is readily visible.
Within the green matrix you can see the fine elastic fibres which give this
cartilage its elastic properties. The elastic fibres may form dense masses
in which individual fibres are difficult to distinguish. The staining of these
masses of fibres may appear more reddish than dark-violet.
A change of the colour of the stain in intensely stained
tissue areas is called "metachromatic staining".
Draw and label a small section of elastic cartilage.
Depending on the quality of tissue preservation on your
slide, it may be possible to identify the
types of epithelia present in the section. It wouldn't hurt trying.


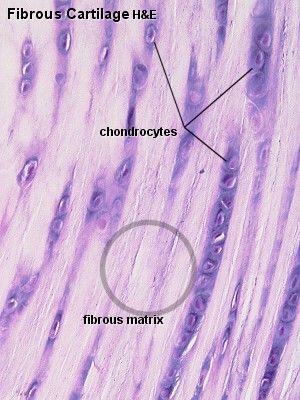
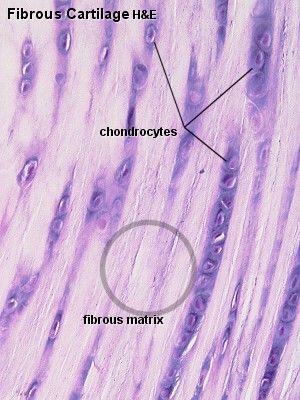
- Suitable Slides
- sections of intervertebral
discs or articular discs - H&E,
van Gieson
Fibrous Cartilage, Intervertebral Disc, sheep, H&E
and Articular Disc, rabbit, H&E
The fibrous cartilage forming the intervertebral discs
varies in appearance from the center of the disc (the nucleus pulposus) the
the periphery of the disc (the anulus fibrosus). Centrally, the fibrous matrix
is very loose. The jelly-like consistency of the central part allows the intervertebral
discs to function as a shock absorber. Towards the periphery, the fibrous
matrix is organised into layers. It is often visible that the fibres of different
layers are oriented at angles to each other - similar to the orientation of
the thread in radial tires. Chondrocytes are very flattened in the periphery
and may be difficult to find.
Midway between periphery and center of the intervertebral disc, chondrocytes
are scattered singly or in small isogenous groups in the dense fibrous matrix
of the cartilage. If you take a close look at the cells you will see that
their appearance actually resembles that of chondrocytes in other types of
cartilage - their characteristic appearance distinguishes fibrous cartilage
preparations from connective tissues. The very regular arrangement of the
fibres in the articular disc may initially let you guess at dense regular
connective tissue. Isogenous groups of chondrocytes again identify the tissue
as fibrous cartilage.
Draw a small section of the fibrous cartilage, including
(if possible) a group of chondrocytes.

- is a specialised form of hyaline cartilage.
- transforms the articulating ends of the bones into lubricated, wear-proof, slightly compressible surfaces, which exhibit very little friction.
- is not surrounded by a perichondrium and is partly vascularised.
- is, depending on the arrangement of chondrocytes and collagenous fibres, divided into several zones:
Tangential layer-
Chondrocytes are rather small and flattened parallel to the surface. The most superficial part (lamina splendens) is devoid of cells. Collagen fibres in the matrix of the tangential layer are very fine. They run parallel to the surface of the cartilage.
Similar to the collagen fibres of the skin, the general orientation of collagen fibres in articular cartilage is determined by tensile and compressive forces at the articulating surfaces.
- Transitional zone
-
The chondrocytes are slightly larger, are round and occur both singly and in isogenous groups. Collagen fibres take an oblique course through the matrix of the transitional zone.
- Radial zone
-
Fairly large chondrocytes form radial columns, i.e. the stacks of cells are oriented perpendicular to the articulating surface. The course of the collagen fibres follows the orientation of the chondrocyte columns.
- Calcified cartilage layer
-
It rests on the underlying cortex of the bone. The matrix of the calcified cartilage layer stains slightly darker (H&E) than the matrix of the other layers.
The main source of nourishment for articular cartilage is the synovial fluid,
which fills the joint cavity. Additional small amounts of nutrients are derived
from blood vessels that course through the calcified cartilage close to the
bone.
Living chondrocytes have been found in small pieces
of cartilage floating in the joint cavity after damage to the articular cartilage.
Osteoarthritis, the slow progressive degeneration of articular
cartilage, is the most common joint disease. It may be caused by persistent
and abnormally high loads on the joint surfaces, which initially result in
the loss of proteoglycans and chondrocytes from the articulating surface of
the cartilage. Subsequently, the cartilage may crack (fibrillate), erode and
expose the underlying bone.
Due to the fairly poor access of nutrients to the chondrocytes they may atrophy in deep parts of thick cartilage. Water content decreases and small cavities arise in the matrix, which often leads to the calcification of the cartilage. This further compromises nutrition. The chondrocytes may eventually die, and the cartilage is gradually transformed to bone.
Chondrogenic activity of the perichondrium is limited to the period of active
growth before adulthood. Although chondrocytes are able to produce matrix
components throughout life, their production can not keep pace with the repair
requirements after acute damage to hyaline or articular cartilage. If these
cartilages are injured after the period of active growth, the defects are
usually filled by connective tissue or fibrous cartilage. The extracellular
matrix of these "repair tissues" is only poorly integrated with
the matrix of the damaged cartilage.
Fortunately, cartilage is rather well suited for transplantation - the metabolism of the chondrocytes is rather slow, the antigenic power of cartilage is rather low, and it is difficult, if not impossible, for antibodies or cells of the immune system to diffuse through the matrix into the cartilage.
![]() .
.