Blood is sometimes considered to be a fluid connective tissue
because of the mesenchymal origin of its cells and a low ratio of
cells to liquid intercellular substance, the blood plasma. In human adults about 5 l of blood
contribute 7-8 % to the body weight of the individual. The
contribution of red blood cells (erythrocytes) to the total volume of the blood
(haematocrit) is about 43%.
Erythrocytes are the dominant (99%) but not the only type of cells in the
blood. We also find leucocytes and, in addition,
blood platelets. Cells in the blood are also
being referred to as the formed elements of the blood.
Erythrocytes and blood platelets perform their functions exclusively in the
blood stream. In contrast, leucocytes reside only temporarily in the blood
and leave the blood stream through the walls of capillaries and venoles and
enter either connective or lymphoid tissues.
Erythrocytes do not contain a nucleus. They do contain haemoglobin, which
fills almost the entire cytoplasm. Erythrocytes are unable to move actively,
but they are remarkably elastic and can withstand deformation. They are typically
biconcave disks although their shape is influenced by osmotic forces. The
average diameter of the disk is ~7 µm. Since erythrocytes can be found
in the vast majority of histological sections - in small numbers even in perfused
tissues - they will often allow us to estimate the size of other structures
or cells. Mature erythrocytes do not contain organelles, and their cytoplasm
looks fairly homogenous - even in the EM.
At high magnification some granularity may be visible in EM images.
The granular appearance is caused by haemoglobin molecules. Early foetal erythrocytes
(up to the 4th month of gestation) are larger than "adult" erythrocytes, and
they are nucleated. The latter feature they share with erythrocytes of other
animal classes (e.g. birds).
Functions
Erythrocytes function in the transport of oxygen. Haemoglobin, the oxygen binding
protein in erythrocytes, contributes about 30% of the weight of an erythrocyte.
The lifespan of an erythrocyte in the bloodstream is 100-120 days.
About 5x1011 erythrocytes are formed/destroyed
each day.
- Suitable
Slides
 blood
smear - Leishman, Wright's, Giemsa or
May-Grünwald-Giemsa stains
blood
smear - Leishman, Wright's, Giemsa or
May-Grünwald-Giemsa stains
?
Where to look for cells in a blood smear
The density of cells varies across the smear. Cells will be "heaped and
piled" close to the point were the drop of blood was placed on the slide.
White blood cells appear shrunken, and some types are difficult to distinguish
from each other. There are fewer cells close to the tip of the smear. In this
region, white blood cells are sometimes damaged and erythrocytes may be deformed.
The best viewing area is between these two regions. Where it is located exactly
and how wide it is will depend on the smear, but the middle of the smear is
a good starting point.
 Blood Smear, human - Leishman
stain
Blood Smear, human - Leishman
stain
How does the shape of the erythrocyte facilitate its
function? How would you expect an erythrocyte to look like if it is in an
extracellular fluid of very low or very high osmotic pressure?
Identify and draw a few erythrocytes.
It is a good idea to do one large composite drawing for all
types of blood cells.
Leucocytes can be further subdivided into granular leucocytes, i.e. neutrophils,
basophils and eosiniphils, and non-granular leucoctes, i.e. monocytes and
lymphocytes.
In healthy individuals the relative numbers of circulating
leucocyte types are quite stable. A differential leucocyte count would typically produce the following cell frequencies (numbers in parentheses are the range of normal frequencies reported in different texts):
- ~ 60% neutrophils (50% - 70%)
- ~ 3% eosinophils (>0% - 5%)
- ~ 0.5% basophils (>0% - 2%)
- ~ 5% monocytes (1% - 9%)
- ~ 30% lymphocytes (20% - 40%)
Changes in their relative numbers indicate that something abnormal is happening
in the organism. For example, a larger than usual number of neutrophils (neutrophilia)
would indicate an acute or chronic infection. The number of basophils and
eosinophils may increase (eosinophilia or basophilia)
as a consequence of allergic disorders.
Granular Leucocytes
Granular leucocytes are all approximately the same size - about 12-15 µm
in diameter. Their nuclei form lobes, and nucleoli cannot be seen. The number
of nuclear lobes varies according to cell type. All granulocytes are motile.
The term granulocytes refers to the presence of granules in the cytoplasm
of these cells. The granules correspond to secretory vesicles and lysosomes.
Specific granules are the granules which
are only found in one particular type of granulocytes.
- Neutrophil granulocytes
(or neurophils)
-
have a very characteristic nucleus. It is divided into 3-5 lobes which are connected by thin strands of chromatin.
The number of lobes increases with cell age. Up to 7 lobes can be found
in very old neutrophils (hypersegmented cells).
Neutrophils (like all other granulocytes, monocytes and lymphocytes)
contain all the organelles that make up a typical cell. In addition to
the usual complement of organelles, they also contain two types of granules.
Primary granules (or A granules) contain lysosomal enzymes and are likely
to be primary lysosomes, although they are larger (0.4 µm) than the "ordinary" primary lysosome. Secondary
granules (or B granules), the specific
granules of the neutrophils, contain enzymes with strong bactericidal
actions. The specific granules of neutrophils stain only weakly
if they are at all visible - they are "neutral", hence the term neutrophil.
Functions
Neutrophils play a central role in inflammatory processes. Large numbers
invade sites of infection and begin to phagocytose tissue debris and foreign
bodies, e.g. bacteria. They are the first wave of cells invading sites
of infection, and their phagocytotic activity is stimulated if invading
microorganisms are "tagged" with antibodies (or opsonised).
Neutrophils cannot replenish their store of granules. The cells die once
their supply of granules has been exhausted. Dead neutrophils and tissue
debris are the major components of pus. Their lifespan is only about one
week.
Lost neutrophils are quickly replenished from
a reserve population in the bone marrow. Because they are younger, their
nuclei have fewer lobes than the "average" neutrophil. A high proportion
of neutrophils with few nuclear lobes indicates a recent surge in their
release from the bone marrow.
- Suitable
Slides
- see lab section on erythrocytes
 Blood Smear, human - Leishman
stain
Blood Smear, human - Leishman
stain
Neutrophil granulocytes are easy to find. They are the most frequent
type of white blood cells, and the complex shape of their nucleus identifies
them unequivocally. In darkly stained smears it is possible to see some faintly
purple, very small granules in the cytoplasm. These granules represent the
primary granules of neutrophils.
Have a close look at the nucleus of a number of neutrophils,
and make a qualified
guess at the gender of the individual, which donated blood for the slides.
Identify and draw one or two neutrophil granulocytes.
How the neutrophils and other leucocytes exactly
will look like depends somewhat on how the stain turned out. In some batches
(B2) nuclei are dark and crisp, and the cytoplasm is well demarcated. In other
batches (B1) nuclei and cytoplasm are lighter and their boundaries are less
well defined. While the morphology appears clearer in the darker stained smears,
it will usually be more difficult to identify eosinophils and basophils (see
below).
- Eosinophil granulocytes (or
eosinophils)
-
Their nucleus usually has only two lobes. Almost all of the cytoplasm appears
filled with the specific granules of the eosinophils. As the term "eosinophil"
indicates, these granules are not neutral but stain red or pink when eosin or
a similar dye is used in the staining process. Aside from the usual complement
of organelles eosinophils contain some large rounded vesicles (up to 1 µm) in their cytoplasm. These granules
correspond to the eosinophilic grains that we see in the light microscope. The
specific granules contain, in addition to enzymes that otherwise are found in
lysosomes, an electron-dense, proteinaceous crystal. This crystal is composed
of major basic protein
(MBP)
Functions
The presence of antibody-antigen complexes stimulates the immune system. Eosinophils
phagocytose these complexes and this may prevent the immune system from "overreacting".
Their granules also contain the enzymes histaminase
and arylsufatase. These enzymes break down histamine
and leukotrienes, which again may dampen the effects of their release by basophils
or mast cells. MBP, which can also function as a cytotoxin, and its release by
eosinophils may be involved in the response of the body against parasitic infections,
which are accompanied by an increase in the number of eosinophils.
- Suitable Slides
- see lab section on erythrocytes
Blood Smear, human - Leishman stain
Eosinophils and basophils may initially be difficult to distinguish
- in particular in darker smears. If you see them side by side in your drawing
the difference between them should become apparent. Chances are 6:1 that the
you find an eosinophil before you find a basophil. The two lobes of the nucleus
of eosinophils are usually well-defined and of about equal size. The nucleus
is embedded in a cytoplasm crowded with granules, which seem to form a solid
mass in the cell. The 2-3 nuclear lobes of basophils are not as well defined
as those of eosinophils, granules are not as numerous as in eosinophils and
pretty much all of them can be identified "as individuals" rather
than the dense mass they form in eosinophils.
Note that eosinophils and basophils are much easier
to distinguish in B1. In B2, the difference in the staining of their of granules
is not as pronounced, and the nuclei do not stand out as clear as in B1.
Identify, draw and label an eosinophil and a basophil.


- Basophil granulocytes (or basophils)
-
Basophilic granulocytes have a 2 or 3 lobed nucleus. The lobes are usually
not as well defined as in neutrophilic granulocytes and the nucleus may
appear S-shaped. The specific granules of basophils are stained deeply
bluish or reddish-violet. Their colour corresponds closely to the colour of the nucleus which
sometimes is difficult to see amongst or behind the granules. The
granules are not as numerous as those in eosinophils. The specific granules
of basophils (about 0.5 µm) appear
quite dark in EM pictures. They contain heparin, histamine, lysosomal
enzymes and leukotrienes (the latter correspond
to the slow-reacting substance of anaphylaxis
or SRS-A).
Functions
Heparin and histamine are vasoactive substances. They dilate the blood
vessels, make vessel walls more permeable and prevent blood coagulation.
As a consequence, they facilitate the access of other leucocytes and of
plasma-borne substances of importance for the immune response to the tissue
- e.g. access of neutrophils and antibodies to a site of infection. The
release of the contents of the granules of basophils is receptor-mediated.
Basophils do not produce antibodies, but their plasma membrane contains
receptors which bind antibodies (IgE) produced
by plasma cells (activated B-lymphocytes; see
below). If these antibodies come into contact with their antigens,
they induce the release of the contents of the basophil granules.
-
Monocytes
-
These cells can be slightly larger than granulocytes (about 12-18 µm in diameter). Their cytoplasm stains
usually somewhat stronger than that of granulocytes, but it does not contain
any structures which would be visible in the light microscope using most
traditional stains (a few very fine bluish gains may be visible in some monocytes).
The "textbook" monocyte has a C-shaped nucleus. Monocytes contain granules
(visible in the EM) which in appearance and content correspond to the
primary granules of neutrophils, i.e. the granules correspond to lysosomes.
Functions
Once monocytes enter the connective
tissue they differentiate into macrophages. At sites of
infection macrophages are the dominant cell type after the death of
the invading neutrophils. The phagocytose microorganisms, tissue
debris and the dead neutrophils. Monocytes also give rise to
osteoclasts, which are able to dissolve bone. They are of
importance in bone remodelling.
- Suitable Slides
- see lab section on erythrocytes
Blood Smear, human - Leishman stain
Monocytes and lymphocytes definitely look much prettier in darker stained
smears (B2) than in lighter ones (B1) - mainly because of a clearer distinction
between cytoplasm and nucleus. The cell is very likely to be a lymphocyte
if the nucleus is round and surrounded by a narrow rim of cytoplasm. The C-shaped
nucleus of a textbook monocyte may not be easy to find. The nuclei will vary
from a peanut- to a "fat" S-shape in smears. Whatever the shape
of the nucleus, it is usually not lobed, and
it is bound, at least on its concave side, by a wide rim of non-granular cytoplasm.
Note also the light area of monocyte cytoplasm which is often visible close
to the concave surface of the nucleus. The Golgi apparatus is located in the
area. The Golgi apparatus does not stain as well as
the remainder of the cytoplasm and leaves a light "impression" - the phenomenon
is also called a "negative image".
Identify and draw lymphocytes and a monocyte.


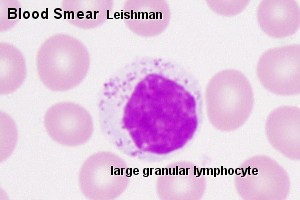
- Lymphocytes
-
These cells are very variable in size. The smallest may be smaller than
erythrocytes (down to ~5 µm in diameter) while the largest may reach
the size of large granulocytes (up to 15 µm in diameter). How much
cytoplasm is discernible depends very much on the size of the lymphocyte.
In small ones, which are the majority of lymphocytes in the blood, the
nucleus may appear to fill the entire cell. Large lymphocytes have a wider
rim of cytoplasm which surrounds the nucleus. Both
the nucleus and the cytoplasm stain blue (and darker than most other cell
types in the blood). The typical lymphocyte only contains the usual
complement of cellular organelles. The appearance of lymphocytes may change
drastically when they are activated (see below).
Functions
Most lymphocytes in the blood stream belong to either the group of B-lymphocytes
(~5%) or the group of T-lymphocytes (~90%).
Unless they become activated, the two groups can not easily be distinguished
using routine light or electron microscopy.
Upon exposure to antigens by antigen-presenting cells (e.g. macrophages)
and T-helper cells (one special group of T-lymphocytes) B-lymphocytes differentiate into antibody producing plasma
cells. The amount of cytoplasm increases and RER fills a
large portion of it.
T-lymphocytes represent the "cellular arm" of the immune response (cytotoxic
T cells) and may attack foreign cells, cancer cells or cells infected
by a virus.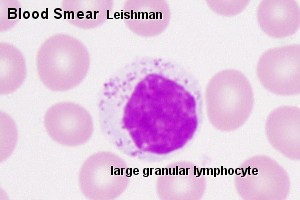
T-lymphocytes and B-lymphocytes form the vast majority
of lymphocytes in the blood stream, but they do not add up to 100%, and
they ususally are small lymphocytes. The much less frequent medium-sized
or large lymphocytes may represent e.g.
- natural killer (Nk-) cells which belong to
the group of large granular lymphocytes, or
- haemopoietic stem cells
of which a few will be circulating in the blood stream.
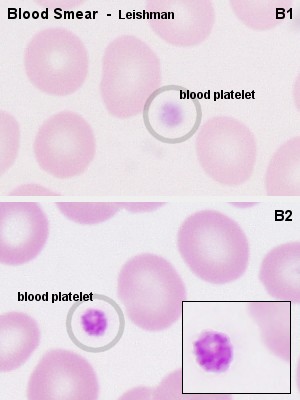
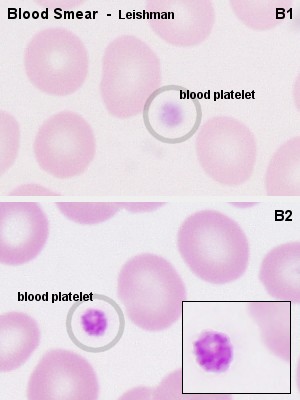
Blood platelets (or thrombocytes)
do not contain a nucleus. Unlike erythrocytes, which also lack a nucleus,
the blood platelets of mammals have never been nucleated cells. Instead, blood platelets are fragments of the cytoplasm of very large
thrombocyte precursor cells, megakaryocytes. Like other cells involved
in the formation in blood cells, megakaryocytes are found in the bone marrow.
Platelets are about 3 µm long but appear somewhat smaller in the microscope.
This is because their cytoplasm is divided into two zones: an outer hyalomere,
which hardly stains, and an inner granulomere,
which contains bluish staining granules. These granules are usually not individually visible with the
highest magnification on your microscope, and the granulomere appears more
or less homogenously blue.
In addition to different types of vesicles
(i.e. the granules), mitochandria, ribosomes, lysosomes and a
little ER are present in the thrombocyte granulomere. Different types
of vesicles contain either serotonin
(electron-dense delta granules; few) or compounds important for blood
coagulation (alpha granules - they also contain platelet-derived growth
factor (PDGF) which may play a role in the
repair of damaged tissue). The hyalomere contains cytoskeletal fibres,
which include actin and myosin.
Functions
Platelets assist in haemostasis, the arrest of bleeding. Serotonin is a potent
vasoconstrictor. The release of serotonin from thrombocytes, which adhere
to the walls of a damaged vessels, is sufficient to close even small arteries.
Platelets, which come into contact with collagenous fibres in the walls of
the vessel (which are not usually exposed to the blood
stream), swell, become "sticky" and activate other platelets to undergo
the same transformation. This cascade of events results in the formation of
a platelet plug (or platelet thrombus). Finally,
activating substances are released from the damaged vessel walls and from
the platelets. These substances mediate the conversion of the plasma protein
prothrombin into thrombin. Thrombin catalyzes
the conversion of fibrinogen into fibrin, which polymerizes into fibrils
and forms a fibrous net in the arising blood clot. Platelets captured in the
fibrin net contract leading to clot retraction, which
further assists in haemostasis.
Blood coagulation is a fairly complex process, which involves a
large number of other proteins and messenger substances.
Deficiencies in any one of them, either inherited or acquired, will
lead to an impairment of haemostasis.
- Suitable Slides
- blood platelets (thrombocytes)
: see lab section on erythrocytes
megakaryoblasts and megakaryocytes: see
lab section on haemopoiesis
 Blood Smear, human - Leishman
stain
Blood Smear, human - Leishman
stain
In lightly stained smears (B1), blood platelets will appear like light
blue, fairly ill-defined specks between the other blood cells. In darker smears
(B2), you will be able to see that the blue specks are formed by an accumulation
of small bluish grains, the granules of the blood platelets.
Identify and include a platelet in one of your other drawings.
Red Bone Marrow, rabbit - H&E
The marrow cavity of this bone is filled with red
bone marrow. H&E is not the method of choice for looking at haemopoietic
cells, but a few of the numerous named types or broader groups can actually
be recognized.
Precursors of platelets are the haemopoietic cells easiest to find
in red bone marrow. The very dark and large megakaryoblast and the even larger
but light megakaryocytes are clearly visible even at low magnifications.
Identify and draw a megakaryocyte and megakaryoblast.


During foetal development, the formation of blood cells (haemopoiesis) commences in wall of the yolk sac. After the
second month of foetal development, the liver,
and, slightly later, the spleen, become the dominant sites of haemopoiesis.
From the 6th month, and dominating from the 7th month onwards, the formation
of blood cells occurs in bone marrow, which is the major site of haemopoiesis
in normal adult humans.
Yellow bone marrow, which harbours mainly adipocytes, dominates in the hollow
of the diaphysis of adult long bones. Haemopoiesis occurs in red
bone marrow, which is typically found between the trabeculae of spongy
bone. Both age and demands on haemopoiesis may effect the relative amounts
of red and yellow bone marrow. Haemopoietic cells surround the vascular sinusoids
and are supported by reticular connective tissue. In addition to the endothelial
cells of the sinusoids and the reticulocytes of the connective tissue, macrophages
are frequent in red bone marrow.
Haemopoietic Cells
The basis of haemopoiesis is a small population of self-replicating stem cells, which ultimately
can generate all types of blood cells. Their progeny may develop
into either lymphocytic stem cells
or pluripotent haemal stem cells (colony-forming unit -
stem cell - CFU-S). The
latter type gives rise to stem cells which can form the major
groups of blood cells other than lymphocytes. Depending on their progeny it is possible to
differentiate
-
burst-forming unit of the
erythroid line (BFU-E),
-
colony-forming unit -
granulocytes and macrophages
(CFU-G/M), and
- colony-forming
unit - megakaryocytes
(CFU-Mk).
-
Erythrocytes
- The first identifiable stage of erythropoiesis is the proerythroblast - a large, slightly basophilic cell,
which contains a large, lightly stained nucleus. Proerythroblasts proliferate
to generate a sequence of cells which show a gradual decrease in size and
condensation of their chromatin. They are named
after changes in the staining characteristic of their cytoplasm (basophilic
erythroblast, polychromatophilic and orthochromic normoblasts). The
nucleus is finally extruded from the normoblast. The cell enters circulation
as a reticulocyte, which still contains
some organelles. Reticulocytes remain for a few days in either the bone
marrow or the spleen to mature to erythrocytes.
-
Granulocytes
- Myeloblast appear light-microscopically similar
to proerythroblast. They proliferate to generate promyelocytes.
Promyelocytes begin to accumulate non-specific granules, but they are still
able to divide. The maturation of their progeny, the myelocytes,
is characterised by the accumulation of specific granules and changes in
nuclear morphology. Metamyelocytes have a
C-shaped nucleus.
-
Thrombocytes
- are, as mentioned above, fragments of the cytoplasm of
megakaryocytes. Megakaryocytes are very large cells (up to 160
µm), which contain very large, highly lobulated, polyploid
nuclei. Megakaryocytes are in turn the product of the
differentiation of basophilic megakaryoblasts.
The nomenclature employed for haemopoietic cells (but
not the number of stages recognized) is somehwat variable across texts.
Note also that these cell types refer to stages of development along a morphologically
more or less continuous spectrum.
Precursors of blood cells which are
usually only found in the bone marrow can be found in peripheral blood in
a variety of pathological conditions.
If a Rh-negative mother has been
immunised by erythrocytes of a Rh-positive foetus, a condition called Erythroblastosis fetalis may develop during subsequent
pregnancies. It would show itself in the foetus or newborn by the presence
of erythrocyte precursors in peripheral blood - although other, more severe
symptoms should be obvious. Chronic myeloid leukemia is another condition
- in this case showing itself by the presence of all types of granulocyte
precursors in peripheral blood.
- Suitable Slides
- sections of red bone marrow
- H&E or a bone marrow smear - Leishman,
Wright's, Giemsa or May-Grünwald-Giemsa stains
Red Bone Marrow, rabbit - H&E
Most of the haemopoietic cells visible will be of the erythroblastic
line. The only cell type of this line which is easy to distinguish in H&E
stained sections are normoblasts.
A very condensed nucleus is seen in late (orthochromic)
normoblast. Granulocyte and erythrocyte precursors will mostly intermingle,
but may be distinguished by nuclear morphology and/or size. A bent nucleus
is found in metamyelocytes - this shape is very pronounced in the last, immature
form of neurophils, which are also called stab or band cells. If the cell
(1) is large, with a distinct "clearing" in the otherwise pink cytoplasm and
(2) has an ovoid or slightly indented nucleus, it is likely to be a myelocyte.
Cells with large light nuclei and almost unstained cytoplasm are either reticulocytes
or macrophages.
Macrophages are frequently associated with normoblasts,
and together these cells form erythroblastic islands. The name for macrophages
in these islands, nurse cells, may tell you a bit about their function in
addition to the scavenging of the expelled nuclei.
Identify normoblasts, myelocytes and metamyelocytes and
include them in your drawing of the megakaryocyte/blast.
If you still have some time and are desperate to get frustrated,
try to hunt up a nice basophilic erythroblast - a basophilic cell with homogenously
staining nucleus that is somewhat smaller than the nuclei of granulocyte-precursors.